
-
By Code 9 Group
- In RCM Services
The Future of Healthcare Revenue Cycle Management
Medical practices seeking financial wellness can no longer afford to be without innovative solutions such as Artificial Intelligence (AI) in the provision of healthcare Revenue Cycle Management (RCM) services. With increased accuracy and responsiveness, higher reimbursements, and a more efficient patient experience, the medical billing and money turnover process within the context of healthcare facilities is becoming increasingly revolutionized through the current use of AI.
What Is Revenue Cycle Management?
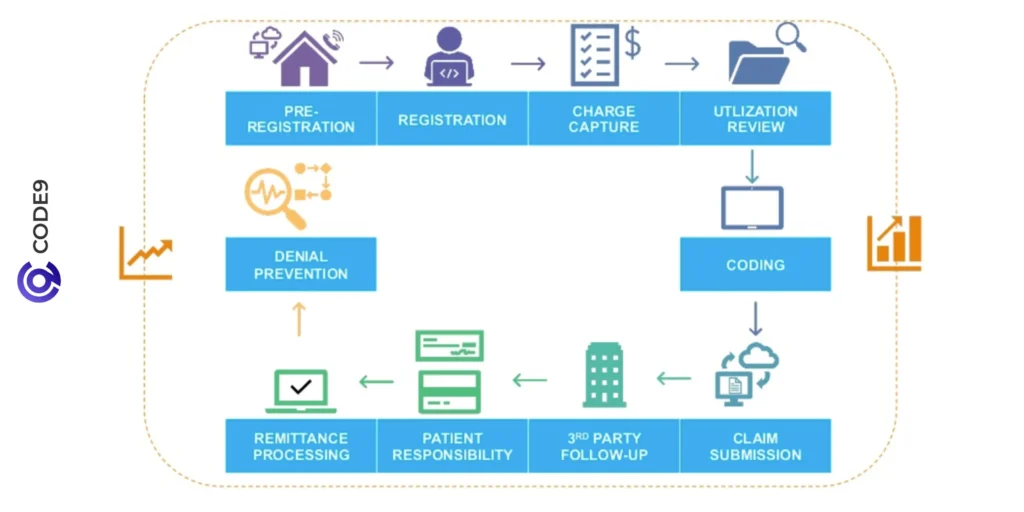
In simplest terms, revenue cycle management is an activity that healthcare providers undertake in monitoring a patient care experience, starting with the initial registration to the final payment. It encompasses all activity tied to confirming insurance coverage and coding diagnoses, and things like billing and handling denials.
How does revenue cycle management work?
It starts with the scheduling of patients, and it ends with when the provider gets full payment of the services. The process of insurance verification, charge capture, claim submission, payment posting, and collection of fees are all individual parts of the financial puzzle. Practices exposed to lack of a quality system are susceptible to delays in payment, bill errors, and non-adherence.
The use of AI in Revenue Cycle Management within Healthcare
Revenue cycle management healthcare is one area in which AI is making headway by automating rote work and generating predictive analytics. With traditional workflow, manual data recording may result to coding mistakes, uncollected charges, delayed reimbursements. These risks are greatly mitigated with the help of AI. Considering the example of the claims care revenue cycle management it is possible to suppose that in it the AI will be able to scan patient records and propose codes that should be applied, and the accuracy is going to be higher, and the size of denials is going to be reduced. It is also able to predict which of the claims are most likely to be rejected and also indicate the same before submitting. The result? A quicker and clever billing cycle at fewer hurdles.

Why Medical Practices Need RCM Technology
The current healthcare providers are facing a situation where the administrative duties are higher than ever. Billing can be daunting as far as changes in regulations or even payer requirements are different. That is the reason why numerous practices are also outsourcing to a revenue cycle management service provider that provides AI-guided tools. By outsourcing to the correct partner, practice compliance will be maintained with a steady cash flow. AI improves efficiency through minimizing human error, better handling of denials, and faster collections, as well as allowing the providers to devote more of their time to patients.
The Increasing Demand for Revenue Cycle Management in Dubai
The need to use intelligent RCM solutions is increasing rapidly on a global scale, with revenue cycle management Dubai being a perfect example of the evolution. The healthcare facilities in the UAE are facing immense pressure to address the international compliance standards, at the same time streamlining the billing processes. The RCM solutions based on AI will provide Dubai-based providers with tools to simplify their claim processing, improve revenue integrity, and promote more successful patient outcomes in a high-growth healthcare market.
Benefits of AI-Driven Claims Care Revenue Cycle Management
Implemented in the right way, AI does not remove staff; it makes their lives more efficient. Your billing team will have time to work on more valuable tasks and automation takes care of things that are repetitive. The inclusion of AI in the claims care revenue cycle management has a lot of advantages:
Quicker settlement of claims: The whole process, which includes pre-authorization and payment posting, is accelerated with the help of AI.
Reduced denials: Predictive participatory instruments examine previous rejections and errors in claims before it is submitted.
Improved compliance: The AI systems also keep abreast with the payer regulations, and the practices can avoid audits and penalties.
Patient transparency: Automated billing estimates and reminders enhance fiscal finances amongst patients.
Selecting a Proper Revenue Cycle Management Service Provider
The key to the success of AI-powered RCM is, accordingly, its choice of a competent provider of revenue cycle management services. Seek a team that will be professional regarding both technology and care. The best provider has custom solutions that suit the magnitude, specialty, and location of your practice. Being a small clinic or multi-specialty group, you require services that scale with your demands. Software is not all that the right partner will provide; it will also bring peace of mind, whether in the form of claims care revenue cycle management or the full-service billing operation.
Advance Forward with Code9 Group
Code9 Group is an all-in-one revenue cycle management service provider that offers the best AI-driven solutions. Catapulting local practice to international healthcare centers, such as our internationally renowned revenue cycle management centers in Dubai, we provide compliant, intelligent, and custom-made RCM support. We will take charge of the billing, and you get to attend to the care. Contact us to learn more about the future of revenue cycle management in healthcare; smart, simple, and effective.
Conclusion
AI is not only trendy but also a new support of healthcare Revenue Cycle Management (RCM) services. With the trend of moving to value-based care and more rigorous adherence, automation will be even more needed. Using smart RCM will enable medical practices to establish sustainable enterprises long into the future in both financial and operations-based aspects.